What Are The Causes Of Severs Disease?
Sever disease refers to a calcaneal apophysitis (an inflammation of the apophysis of the heel) which occurs in children and young adolescents. It typically presents in active young children (especially ones who engage in jumping and running sports).
Causes
The foot is one of the first body parts to grow to full size. During the time of growth, bones grow faster than muscles and tendons. This results in the muscles and tendons becoming tight. The strongest tendon that attaches to the heel is the Achilles Tendon. It attaches to the back of the heel at the site of the growth plate, and during sports activities it pulls with great force on the growth plate. If this pull by the tight Achilles Tendon (calf muscle) continues for long periods of time, the growth plate may become inflamed and painful. If exertive activities continue, Sever's Disease may result.
Symptoms
The patient complains of activity related pain that usually settles with rest. On Examination the heel bone - or calcaneum - is tender on one or both sides. The gastrocnemius and soleus muscles (calf muscles) may be tight and bending of the ankle might be limited because of that. Foot pronation (rolling in) often exacerbates the problem. There is rarely anything to see and with no redness or swelling and a pain that comes and goes mum and dad often wait before seeking advice on this condition. The pain may come on partway through a game and get worse or come at the end of the game. Initially pain will be related only to activity but as it gets worse the soreness will still be there the next morning and the child might limp on first getting up.
Diagnosis
Sever disease is most often diagnosed clinically, and radiographic evaluation is believed to be unnecessary by many physicians, but if a diagnosis of calcaneal apophysitis is made without obtaining radiographs, a lesion requiring more aggressive treatment could be missed. Foot radiographs are usually normal and the radiologic identification of calcaneal apophysitis without the absence of clinical information was not reliable.
Non Surgical Treatment
Treatment includes modifying activities and resting to reduce pain and inflammation and take pressure off the growth center. Ice can also be very helpful in relieving symptoms, as well as anti-inflammatory medication. A physical therapy program should be initiated to stretch tight calf muscles and strengthen the ankle muscles to relieve tension on the growth center. Shoes with padded heel surfaces and good arch support can decrease pain. Cleats may need to be avoided for some time to help reduce symptoms. The doctor may also recommend gel heel cups or supportive shoe inserts.
Recovery
With proper care, your child should feel better within 2 weeks to 2 months. Your child can start playing sports again only when the heel pain is gone. Your doctor will let you know when physical activity is safe.
Causes And Treatment
Overview
For many adults, years of wear and tear on the feet can lead to a gradual and potentially debilitating collapse of the arch. However, a new treatment approach based on early surgical intervention is achieving a high rate of longterm success. Based on results of clinical studies of adults with flat feet, we now believe that reconstructive surgery in the early stages of the condition can prevent complications later on. Left untreated, the arch eventually will collapse, causing debilitating arthritis in the foot and ankle. At this end stage, surgical fusions are often required to stabilize the foot. 
Causes
Overuse of the posterior tibial tendon is often the cause of PTTD. In fact, the symptoms usually occur after activities that involve the tendon, such as running, walking, hiking, or climbing stairs.
Symptoms
At first you may notice pain and swelling along the medial (big toe) side of the foot. This is where the posterior tibialis tendon travels from the back of the leg under the medial ankle bone to the foot. As the condition gets worse, tendon failure occurs and the pain gets worse. Some patients experience pain along the lateral (outside) edge of the foot, too. You may find that your feet hurt at the end of the day or after long periods of standing. Some people with this condition have trouble rising up on their toes. They may be unable to participate fully in sports or other recreational activities.
Diagnosis
Clinicians need to recognize the early stage of this syndrome which includes pain, swelling, tendonitis and disability. The musculoskeletal portion of the clinical exam can help determine the stage of the disease. It is important to palpate the posterior tibial tendon and test its muscle strength. This is tested by asking patient to plantarflex and invert the foot. Joint range of motion is should be assessed as well. Stiffness of the joints may indicate longstanding disease causing a rigid deformity. A weightbearing examination should be performed as well. A complete absence of the medial longitudinal arch is often seen. In later stages the head of the talus bone projects outward to the point of a large "lump" in the arch. Observing the patient's feet from behind shows a significant valgus rotation of the heel. From behind, the "too many toes" sign may be seen as well. This is when there is abducution of the forefoot in the transverse plane allowing the toes to be seen from behind. Dysfunction of the posterior tibial tendon can be assessed by asking the patient to stand on his/her toes on the affected foot. If they are unable to, this indicates the disease is in a more advanced stage with the tendon possibly completely ruptured.
Non surgical Treatment
A painless flatfoot that does not hinder your ability to walk or wear shoes requires no special treatment or orthotic device. Other treatment options depend on the cause and progression of the flatfoot. Conservative treatment options include making shoe modifications. Using orthotic devices such as arch supports and custom-made orthoses. Taking nonsteroidal anti-inflammatory drugs such as ibuprofen to relieve pain. Using a short-leg walking cast or wearing a brace. Injecting a corticosteroid into the joint to relieve pain. Rest and ice. Physical therapy. In some cases, surgery may be needed to correct the problem. Surgical procedures can help reduce pain and improve bone alignment. 
Surgical Treatment
Good to excellent results for more than 80% of patients have been reported at five years' follow up for the surgical interventions recommended below. However, the postoperative recovery is a lengthy process, and most surgical procedures require patients to wear a plaster cast for two to three months. Although many patients report that their function is well improved by six months, in our experience a year is required to recover truly and gain full functional improvement after the surgery. Clearly, some patients are not candidates for such major reconstructive surgery.
Adult Aquired Flat Foot Do I Suffer AAF?
Over 60 Million Americans suffer from Adult Acquired Flatfoot (AAF), otherwise known as Posterior Tibial Tendon Dysfunction or PTTD. This condition generally occurs in adults from 40-65 years of age, and it usually only occurs in one foot, not both. The Posterior Tibial (PT) Tendon courses along the inside part of the ankle and underneath the arch of the foot. It is the major supporting structure for the arch. Over time, the tendon becomes diseased, from overuse, and starts to lose it's strength. As a result, the arch begins to collapse, placing further strain on the PT Tendon, leading to further decrease in tendon strength, which causes further collapse of the arch. This is described as a progressive deformity because it will generally get worse over time.

Causes
Causes of an adult acquired flatfoot may include Neuropathic foot (Charcot foot) secondary to Diabetes mellitus, Leprosy, Profound peripheral neuritis of any cause. Degenerative changes in the ankle, talonavicular or tarsometatarsal joints, or both, secondary to Inflammatory arthropathy, Osteoarthropathy, Fractures, Acquired flatfoot resulting from loss of the supporting structures of the medial longitudinal arch. Dysfunction of the tibialis posterior tendon Tear of the spring (calcaneoanvicular) ligament (rare). Tibialis anterior rupture (rare). Painful flatfoot can have other causes, such as tarsal coalition, but as such a patient will not present with a change in the shape of the foot these are not included here.
Symptoms
Posterior tibial tendon insufficiency is divided into stages by most foot and ankle specialists. In stage I, there is pain along the posterior tibial tendon without deformity or collapse of the arch. The patient has the somewhat flat or normal-appearing foot they have always had. In stage II, deformity from the condition has started to occur, resulting in some collapse of the arch, which may or may not be noticeable. The patient may feel it as a weakness in the arch. Many patients initially present in stage II, as the ligament failure can occur at the same time as the tendon failure and therefore deformity can already be occurring as the tendon is becoming symptomatic. In stage III, the deformity has progressed to the extent where the foot becomes fixed (rigid) in its deformed position. Finally, in stage IV, deformity occurs at the ankle in addition to the deformity in the foot.
Diagnosis
Perform a structural assessment of the foot and ankle. Check the ankle for alignment and position. When it comes to patients with severe PTTD, the deltoid has failed, causing an instability of the ankle and possible valgus of the ankle. This is a rare and difficult problem to address. However, if one misses it, it can lead to dire consequences and potential surgical failure. Check the heel alignment and position of the heel both loaded and during varus/valgus stress. Compare range of motion of the heel to the normal contralateral limb. Check alignment of the midtarsal joint for collapse and lateral deviation. Noting the level of lateral deviation in comparison to the contralateral limb is critical for surgical planning. Check midfoot alignment of the naviculocuneiform joints and metatarsocuneiform joints both for sag and hypermobility.
Non surgical Treatment
Footwear has an important role, and patients should be encouraged to wear flat lace-up shoes, or even lace-up boots, which accommodate orthoses. Stage I patients may be able to manage with an off the shelf orthosis (such as an Orthaheel or Formthotics). They can try a laced canvas ankle brace before moving to a casted orthosis. The various casted, semirigid orthoses support the medial longitudinal arch of the foot and either hold the heel in a neutral alignment (stage I) or correct the outward bent heel to a neutral alignment (stage II). This approach is meant to serve several functions: to alleviate stress on the tibialis posterior; to make gait more efficient by holding the hindfoot fixed; and thirdly, to prevent progression of deformity. Devices available to do this are the orthosis of the University of California Biomechanics Laboratory, an ankle foot orthosis, or a removable boot. When this approach has been used, two thirds of patients have good to excellent results.
03.jpg)
Surgical Treatment
Types of surgery your orthopaedist may discuss with you include arthrodesis, or welding (fusing) one or more of the bones in the foot/ankle together. Osteotomy, or cutting and reshaping a bone to correct alignment. Excision, or removing a bone or bone spur. Synovectomy, or cleaning the sheath covering a tendon. Tendon transfer, or using a piece of one tendon to lengthen or replace another. Having flat feet is a serious matter. If you are experiencing foot pain and think it may be related to flat feet, talk to your orthopaedist.
Achilles Tendinitis Treatments And Causes
 Achilles tendonitis is a condition wherein the Achilles tendon, at or near its insertion to back of the heel, becomes inflamed and causes pain. The Achilles tendon is one of the longest and strongest tendons in the body. It is avascular (not supplied with blood vessels) so it can be slow to heal. The Achilles tendon is formed in the lower third of the leg. Two muscles join to form the Achilles tendon, the Gastrocnemius and the Soleus which are commonly referred to as the calf muscle. The Achilles tendon works as an anti-pronator which means it helps to prevent the foot from rolling inward.
Achilles tendonitis is a condition wherein the Achilles tendon, at or near its insertion to back of the heel, becomes inflamed and causes pain. The Achilles tendon is one of the longest and strongest tendons in the body. It is avascular (not supplied with blood vessels) so it can be slow to heal. The Achilles tendon is formed in the lower third of the leg. Two muscles join to form the Achilles tendon, the Gastrocnemius and the Soleus which are commonly referred to as the calf muscle. The Achilles tendon works as an anti-pronator which means it helps to prevent the foot from rolling inward.
Causes
The majority of Achilles tendon injuries are due to overuse injuries. Other factors that lead to Achilles tendonitis are improper shoe selection, inadequate stretching prior to engaging in athletics, a short Achilles tendon, direct trauma (injury) to the tendon, training errors and heel bone deformity. There is significant evidence that people with feet that role in excessively (over-pronate) are at greater risk for developing Achilles tendinitis. The increased pronation puts additional stress on the tendon, therefore, placing it at greater risk for injury.
Symptoms
The primary symptom of Achilles tendon inflammation is pain in the back of the heel, which initially increases when exercise is begun and often lessens as exercise continues. A complete tear of the Achilles tendon typically occurs with a sudden forceful change in direction when running or playing tennis and is often accompanied by a sensation of having been struck in the back of the ankle and calf with an object such as a baseball bat.
Diagnosis
Examination of the achilles tendon is inspection for muscle atrophy, swelling, asymmetry, joint effusions and erythema. Atrophy is an important clue to the duration of the tendinopathy and it is often present with chronic conditions. Swelling, asymmetry and erythema in pathologic tendons are often observed in the examination. Joint effusions are uncommon with tendinopathy and suggest the possibility of intra-articular pathology. Range of motion testing, strength and flexibility are often limited on the side of the tendinopathy. Palpation tends to elicit well-localized tenderness that is similar in quality and location to the pain experienced during activity. Physical examinations of the Achilles tendon often reveals palpable nodules and thickening. Anatomic deformities, such as forefoot and heel varus and excessive pes planus or foot pronation, should receive special attention. These anatomic deformities are often associated with this problem. In case extra research is wanted, an echography is the first choice of examination when there is a suspicion of tendinosis. Imaging studies are not necessary to diagnose achilles tendonitis, but may be useful with differential diagnosis. Ultrasound is the imaging modality of first choice as it provides a clear indication of tendon width, changes of water content within the tendon and collagen integrity, as well as bursal swelling. MRI may be indicated if diagnosis is unclear or symptoms are atypical. MRI may show increased signal within the Achilles.
Nonsurgical Treatment
Most cases of Achilles tendonitis can be treated at home. Here's what to do. Stop doing the activity that led to the injury. Avoid putting stress on your legs and feet, and give your tendon plenty of time to fully recover. Use the RICE formula. Don't exercise for a few days, or try an exercise that doesn't stress your feet, such as swimming. If necessary, your doctor may recommend that you use crutches or wear a walking boot to keep weight off your foot. Apply an ice pack wrapped in a towel or a cold compress to your tendon for 15 minutes or more after you exercise or if you feel pain in the tendon. Use tape or an athletic wrap to keep swelling down and help support and immobilize the tendon. Lie down and raise your foot above the level of your heart, and if possible, try to sleep with your foot elevated. This will help keep the swelling to a minimum. Take anti-inflammatory medications. Pain relievers like ibuprofen can help ease pain and reduce swelling in the affected area. Stretch and exercise your ankles and calf muscles while you recover. Keeping your muscles, tendons, and ligaments strong and flexible will aid in your recovery and help you keep from reinjuring your Achilles tendon. A doctor or a physical therapist can help you come up with a good exercise program. Try a pair of prescription orthotic inserts for your shoes if your doctor thinks it will help. Sometimes orthotics can be helpful. Talk to your doctor or someone trained in fitting orthotics to find out if they might work for you. Achilles tendon surgery is rarely needed. It's usually only done if the tendon breaks, and then only as a last resort after other methods of therapy have been tried. Most cases of Achilles tendonitis will get better on their own with rest and minor treatment.

Surgical Treatment
Occasionally, conservative management of Achilles tendon conditions fails. This failure is more common in older male patients and those with longstanding symptoms, those who persist in full training despite symptoms or those who have uncorrected predisposing factors. In these cases, surgery may be indicated. It should be remembered, however, that the rehabilitation program, particularly for severe Achilles tendon injuries, is a slow, lengthy program. Surgery is only indicated when there is failure to progress in the rehabilitation program. Surgery should not be considered unless at least six months of appropriate conservative management has failed to lead to improvement.
Prevention
Stay in good shape year-round and try to keep your muscles as strong as they can be. Strong, flexible muscles work more efficiently and put less stress on your tendon. Increase the intensity and length of your exercise sessions gradually. This is especially important if you've been inactive for a while or you're new to a sport. Always warm up before you go for a run or play a sport. If your muscles are tight, your Achilles tendons have to work harder to compensate. Stretch it out. Stretch your legs, especially your calves, hamstrings, quadriceps, and thigh muscles - these muscles help stabilize your knee while running. Get shoes that fit properly and are designed for your sport. If you're a jogger, go to a running specialty store and have a trained professional help you select shoes that match your foot type and offer plenty of support. Replace your shoes before they become worn out. Try to run on softer surfaces like grass, dirt trails, or synthetic tracks. Hard surfaces like concrete or asphalt can put extra pressure on the joints. Also avoid running up or down hills as much as possible. Vary your exercise routine. Work different muscle groups to keep yourself in good overall shape and keep individual muscles from getting overused. If you notice any symptoms of Achilles tendonitis, stop running or doing activities that put stress on your feet. Wait until all the pain is gone or you have been cleared to start participating again by a doctor.
What Is Heel Pain

Overview
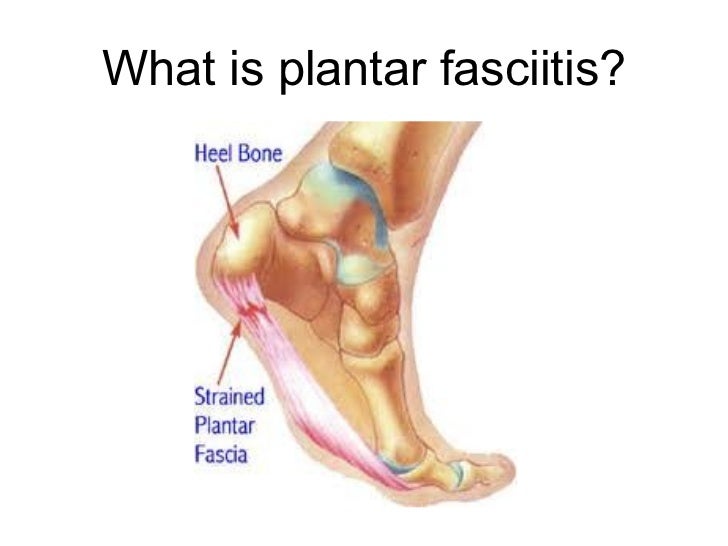
Plantar fasciitis is a common painful disorder affecting the heel and underside of the foot. It is a disorder of the insertion site of plantar fascia on the bone and is characterized by scarring, inflammation, or structural breakdown of the foot’s plantar fascia. It is often caused by overuse injury of the plantar fascia, increases in exercise, weight or age. Although plantar fasciitis was originally thought to be an inflammatory process, newer studies have demonstrated structural changes more consistent with a degenerative process. As a result of this new observation, many in the academic community have stated the condition should be renamed plantar fasciosis.
Causes
Far and away the most common cause of plantar fasciitis in an athlete is faulty biomechanics of the foot or leg. Faulty biomechanics causes the foot to sustain increased or prolonged stresses over and above those of routine ground contacts. Throughout the phase of ground contact, the foot assumes several mechanical positions to dissipate shock while at the same time placing the foot in the best position to deliver ground forces. With heel landing the foot is supinated (ankle rolled out). At mid-stance the foot is pronated (ankle rolled in). The foot is supinated again with toe-off. The supination of the foot at heel strike and toe-off makes the foot a rigid lever. At heel strike the shock of ground contact is transferred to the powerful quads. During toe-off forward motion is created by contraction of the gastroc complex plantar flexing the rigid lever of the foot pushing the body forward.
Symptoms
The main symptom of plantar fasciitis is heel pain when you walk. You may also feel pain when you stand and possibly even when you are resting. This pain typically occurs first thing in the morning after you get out of bed, when your foot is placed flat on the floor. The pain occurs because you are stretching the plantar fascia. The pain usually lessens with more walking, but you may have it again after periods of rest. You may feel no pain when you are sleeping because the position of your feet during rest allows the fascia to shorten and relax.
Diagnosis
Plantar fasciitis is usually diagnosed by your physiotherapist or sports doctor based on your symptoms, history and clinical examination. After confirming your plantar fasciitis they will investigate WHY you are likely to be predisposed to plantar fasciitis and develop a treatment plan to decrease your chance of future bouts. X-rays may show calcification within the plantar fascia or at its insertion into the calcaneus, which is known as a calcaneal or heel spur. Ultrasound scans and MRI are used to identify any plantar fasciitis tears, inflammation or calcification. Pathology tests (including screening for HLA B27 antigen) may identify spondyloarthritis, which can cause symptoms similar to plantar fasciitis.
Non Surgical Treatment
Treatment of heel pain caused by plantar fasciitis begins with simple steps. There are a number of options for treatment of plantar fasciitis, and almost always some focused effort with nonsurgical treatments can provide excellent relief. In rare circumstances, simple steps are not adequate at providing relief, and more invasive treatments may be recommended. Typically, patients progress from simple steps, and gradually more invasive treatments, and only rarely is surgery required.

Surgical Treatment
If treatment hasn't worked and you still have painful symptoms after a year, your GP may refer you to either an orthopaedic surgeon, a surgeon who specialises in surgery that involves bones, muscles and joints, a podiatric surgeon, a podiatrist who specialises in foot surgery. Surgery is sometimes recommended for professional athletes and other sportspeople whose heel pain is adversely affecting their career. Plantar release surgery. Plantar release surgery is the most widely used type of surgery for heel pain. The surgeon will cut the fascia to release it from your heel bone and reduce the tension in your plantar fascia. This should reduce any inflammation and relieve your painful symptoms. Surgery can be performed either as, open surgery, where the section of the plantar fascia is released by making a cut into your heel, endoscopic or minimal incision surgery - where a smaller incision is made and special instruments are inserted through the incision to gain access to the plantar fascia. Endoscopic or minimal incision surgery has a quicker recovery time, so you will be able to walk normally much sooner (almost immediately), compared with two to three weeks for open surgery. A disadvantage of endoscopic surgery is that it requires both a specially trained surgical team and specialised equipment, so you may have to wait longer for treatment than if you were to choose open surgery. Endoscopic surgery also carries a higher risk of damaging nearby nerves, which could result in symptoms such as numbness, tingling or some loss of movement in your foot. As with all surgery, plantar release carries the risk of causing complications such as infection, nerve damage and a worsening of your symptoms after surgery (although this is rare). You should discuss the advantages and disadvantages of both techniques with your surgical team. Extracorporeal shockwave therapy (EST) is a fairly new type of non-invasive treatment. Non-invasive means it does not involve making cuts into your body. EST involves using a device to deliver high-energy soundwaves into your heel. The soundwaves can sometimes cause pain, so a local anaesthetic may be used to numb your heel. It is claimed that EST works in two ways. It is thought to, have a "numbing" effect on the nerves that transmit pain signals to your brain, help stimulate and speed up the healing process. However, these claims have not yet been definitively proven. The National Institute for Health and Care Excellence (NICE) has issued guidance about the use of EST for treating plantar fasciitis. NICE states there are no concerns over the safety of EST, but there are uncertainties about how effective the procedure is for treating heel pain. Some studies have reported that EST is more effective than surgery and other non-surgical treatments, while other studies found the procedure to be no better than a placebo (sham treatment).
What May Cause Plantar Fasciitis

Overview
Plantar fasciitis is a common cause of heel pain in adults. The pain is usually caused by collagen degeneration (which is sometimes misnamed “chronic inflammation”) at the origin of the plantar fascia at the medial tubercle of the calcaneus. This degeneration is similar to the chronic necrosis of tendonosis, which features loss of collagen continuity, increases in ground substance (matrix of connective tissue) and vascularity, and the presence of fibro-blasts rather than the inflammatory cells usually seen with the acute inflammation of tendonitis. The cause of the degeneration is repetitive microtears of the plantar fascia that overcome the body's ability to repair itself.
Causes
The most common cause of plantar fasciitis relates to faulty structure of the foot. For example, people who have problems with their arches, either overly flat feet or high-arched feet, are more prone to developing plantar fasciitis. Wearing non-supportive footwear on hard, flat surfaces puts abnormal strain on the plantar fascia and can also lead to plantar fasciitis. This is particularly evident when one’s job requires long hours on the feet. Obesity may also contribute to plantar fasciitis.
Symptoms
Pain tends to start gradually, often just in the heel, but it can sometimes be felt along the whole of the plantar fascia. The symptoms are initially worse in the morning and mostly after, rather than during, activity. As the condition becomes worse, the symptoms become more persistent.
Diagnosis
Your doctor will check your feet and watch you stand and walk. He or she will also ask questions about your past health, including what illnesses or injuries you have had. Your symptoms, such as where the pain is and what time of day your foot hurts most. How active you are and what types of physical activity you do. Your doctor may take an X-ray of your foot if he or she suspects a problem with the bones of your foot, such as a stress fracture.
Non Surgical Treatment
Heel cups are used to decrease the impact on the calcaneus and to theoretically decrease the tension on the plantar fascia by elevating the heel on a soft cushion. Although heel cups have been found to be useful by some physicians and patients, in our experience they are more useful in treating patients with fat pad syndrome and heel bruises than patients with plantar fasciitis. In a survey of 411 patients with plantar fasciitis, heel cups were ranked as the least effective of 11 different treatments.

Surgical Treatment
The most common surgical procedure for plantar fasciitis is plantar fascia release. It involves surgical removal of a part from the plantar fascia ligament which will relieve the inflammation and reduce the tension. Plantar fascia release is either an open surgery or endoscopic surgery (insertion of special surgical instruments through small incisions). While both methods are performed under local anesthesia the open procedure may take more time to recover. Other surgical procedures can be used as well but they are rarely an option. Complications of plantar fasciitis surgery are rare but they are not impossible. All types of plantar fasciitis surgery pose a risk of infection, nerve damage, and anesthesia related complications including systemic toxicity, and persistence or worsening of heel pain.
Stretching Exercises
You may begin exercising the muscles of your foot right away by gently stretching them as follows. Prone hip extension, Lie on your stomach with your legs straight out behind you. Tighten up your buttocks muscles and lift one leg off the floor about 8 inches. Keep your knee straight. Hold for 5 seconds. Then lower your leg and relax. Do 3 sets of 10. Towel stretch, Sit on a hard surface with one leg stretched out in front of you. Loop a towel around your toes and the ball of your foot and pull the towel toward your body keeping your knee straight. Hold this position for 15 to 30 seconds then relax. Repeat 3 times. When the towel stretch becomes too easy, you may begin doing the standing calf stretch. Standing calf stretch, Facing a wall, put your hands against the wall at about eye level. Keep one leg back with the heel on the floor, and the other leg forward. Turn your back foot slightly inward (as if you were pigeon-toed) as you slowly lean into the wall until you feel a stretch in the back of your calf. Hold for 15 to 30 seconds. Repeat 3 times. Do this exercise several times each day. Sitting plantar fascia stretch, Sit in a chair and cross one foot over your other knee. Grab the base of your toes and pull them back toward your leg until you feel a comfortable stretch. Hold 15 seconds and repeat 3 times. When you can stand comfortably on your injured foot, you can begin standing to stretch the bottom of your foot using the plantar fascia stretch. Achilles stretch, Stand with the ball of one foot on a stair. Reach for the bottom step with your heel until you feel a stretch in the arch of your foot. Hold this position for 15 to 30 seconds and then relax. Repeat 3 times. After you have stretched the bottom muscles of your foot, you can begin strengthening the top muscles of your foot. Frozen can roll, Roll your bare injured foot back and forth from your heel to your mid-arch over a frozen juice can. Repeat for 3 to 5 minutes. This exercise is particularly helpful if done first thing in the morning. Towel pickup, With your heel on the ground, pick up a towel with your toes. Release. Repeat 10 to 20 times. When this gets easy, add more resistance by placing a book or small weight on the towel. Balance and reach exercises, Stand upright next to a chair. This will provide you with balance if needed. Stand on the foot farthest from the chair. Try to raise the arch of your foot while keeping your toes on the floor. Keep your foot in this position and reach forward in front of you with your hand farthest away from the chair, allowing your knee to bend. Repeat this 10 times while maintaining the arch height. This exercise can be made more difficult by reaching farther in front of you. Do 2 sets. Stand in the same position as above. While maintaining your arch height, reach the hand farthest away from the chair across your body toward the chair. The farther you reach, the more challenging the exercise. Do 2 sets of 10. Heel raise, Balance yourself while standing behind a chair or counter. Using the chair to help you, raise your body up onto your toes and hold for 5 seconds. Then slowly lower yourself down without holding onto the chair. Hold onto the chair or counter if you need to. When this exercise becomes less painful, try lowering on one leg only. Repeat 10 times. Do 3 sets of 10. Side-lying leg lift, Lying on your side, tighten the front thigh muscles on your top leg and lift that leg 8 to 10 inches away from the other leg. Keep the leg straight. Do 3 sets of 10.
What Is Heel Pain And The Right Way To Alleviate It
Overview
Plantar fasciitis, also called “heel pain syndrome,” affects approximately 2 million people in the United States each year. Plantar fasciitis can come on gradually as the result of a degenerative process or sudden foot trauma. It can appear in one heel or both. It is generally worse on taking the first few steps in the morning or after prolonged sitting or non-weight-bearing movement. Symptoms can be aggravated by activity and prolonged weight bearing. Obesity, too, is hard on the feet-it can cause plantar pain or it can make that pain worse. The plantar fascia connects the calcaneal tubercle to the forefoot with five slips directed to each toe respectively. Other conditions, such as calcaneal fat pad atrophy, calcaneal stress fracture, nerve entrapment, and rheumatoid arthritis may also cause foot pain. These conditions may be found in combination with plantar fasciitis, or separate from it. A blood test can help pinpoint the cause(s).
Causes
Plantar fasciitis is usually not the result of a single event but more commonly the result of a history of repetitive micro trauma combined with a biomechanical deficiency of the foot. Arthritic changes and metabolic factors may also playa part in this injury but are unlikely in a young athletic population. The final cause of plantar fasciitis is "training errors." In all likelihood the injury is the result of a combination of biomechanical deficiencies and training errors. Training errors are responsible for up to 60% of all athletic injuries (Ambrosius 1992). The most frequent training error seen with plantar fasciitis is a rapid increase in volume (miles or time run) or intensity (pace and/or decreased recovery). Training on improper surfaces, a highly crowned road, excessive track work in spiked shoes, plyometrics on hard runways or steep hill running, can compromise the plantar fascia past elastic limits. A final training error seen in athletics is with a rapid return to some preconceived fitness level. Remembering what one did "last season" while forgetting the necessity of preparatory work is part of the recipe for injury. Metabolic and arthritic changes are a less likely cause of plantar fasciitis among athletes. Bilateral foot pain may indicate a metabolic or systemic problem. The definitive diagnosis in this case is done by a professional with blood tests and possibly x-rays.
Symptoms
The symptoms of plantar fasciitis include pain in the bottom of your foot, especially at the front or centre of the heel bone, pain that is worse when first rising in the morning (called "first-step pain"), when first standing up after any long period of sitting, or after increased levels of activity especially in non-supportive shoes. Seek medical advice about plantar fasciitis if you have heel pain or pain in the bottom of your foot, especially when you get up in the morning, that does not respond to treatment or if there is redness or bruising in the heel.
Diagnosis
After you describe your symptoms and discuss your concerns, your doctor will examine your foot. Your doctor will look for these signs. A high arch, an area of maximum tenderness on the bottom of your foot, just in front of your heel bone. Pain that gets worse when you flex your foot and the doctor pushes on the plantar fascia. The pain improves when you point your toes down. Limited "up" motion of your ankle. Your doctor may order imaging tests to help make sure your heel pain is caused by plantar fasciitis and not another problem. X-rays provide clear images of bones. They are useful in ruling out other causes of heel pain, such as fractures or arthritis. Heel spurs can be seen on an x-ray. Other imaging tests, such as magnetic resonance imaging (MRI) and ultrasound, are not routinely used to diagnose plantar fasciitis. They are rarely ordered. An MRI scan may be used if the heel pain is not relieved by initial treatment methods.
Non Surgical Treatment
Conservative treatment is almost always successful, given enough time. Traditional treatment often includes, rest, NSAIDs, and new shoes or heel inserts. Some doctors also recommend avoiding walking bare-footed. This means you’d have to wear your shoes as soon as you wake up. Certain foot and calf exercises are often prescribed to slowly build strength in the ligaments and muscles that support the arch of the foot. While traditional treatment usually relieves pain, it can last from several months to 2 years before symptoms get better. On average, non-Airrosti patients tend to get better in about 9 months.

Surgical Treatment
Most practitioners agree that treatment for plantar fasciitis is a slow process. Most cases resolve within a year. If these more conservative measures don't provide relief after this time, your doctor may suggest other treatment. In such cases, or if your heel pain is truly debilitating and interfering with normal activity, your doctor may discuss surgical options with you. The most common surgery for plantar fasciitis is called a plantar fascia release and involves releasing a portion of the plantar fascia from the heel bone. A plantar fascia release can be performed through a regular incision or as endoscopic surgery, where a tiny incision allows a miniature scope to be inserted and surgery to be performed. About one in 20 patients with plantar fasciitis will need surgery. As with any surgery, there is still some chance that you will continue to have pain afterwards.